The U.S. Food and Drug Administration (FDA) has approved Wegovy (semaglutide) injection (2.4 mg once weekly) as a new treatment for chronic weight management in adults with obesity or overweight. This marks the first such approval since 2014. The drug is intended for individuals with a body mass index (BMI) of 30 kg/m² or greater or those with a BMI of 27 kg/m² or greater and at least one weight-related condition, such as high blood pressure, type 2 diabetes, or high cholesterol.
Obesity is a growing public health concern, affecting nearly 70% of American adults. It is directly linked to life-threatening conditions such as heart disease, stroke, diabetes, and certain cancers. Research indicates that losing 5% to 10% of body weight through lifestyle changes can significantly reduce cardiovascular risks. The FDA’s approval of Wegovy offers a new tool for those struggling to manage their weight despite diet and exercise efforts.
“This approval provides an additional treatment option for adults with obesity or overweight to incorporate into a comprehensive weight management plan,” said John Sharretts, M.D., deputy director at the FDA’s Center for Drug Evaluation and Research.
Wegovy is a glucagon-like peptide-1 (GLP-1) receptor agonist, a class of drugs that influences hunger and calorie intake. It mimics GLP-1, a hormone that regulates appetite, sending signals to the brain to reduce hunger and food consumption.
The treatment follows a gradual dose escalation over 16 to 20 weeks to minimize gastrointestinal side effects. Patients start with a lower dose before reaching the full 2.4 mg weekly injection.
Wegovy is approved for:
It is not recommended for individuals who:
The FDA’s approval was based on four 68-week clinical trials, three of which were randomized, double-blind, placebo-controlled studies. Over 2,600 patients were treated with Wegovy, while 1,500 received a placebo.
These results demonstrate statistically significant weight loss, reinforcing Wegovy’s potential as an effective intervention for obesity.
Like other GLP-1 receptor agonists, Wegovy carries a risk of gastrointestinal side effects. The most commonly reported symptoms include:
More serious warnings include a boxed warning for thyroid C-cell tumors. The drug should not be used by individuals with:
Additional risks involve pancreatitis, gallbladder disease, kidney injury, increased heart rate, diabetic retinopathy, and potential suicidal thoughts or behaviors. Patients experiencing severe allergic reactions should discontinue use immediately and seek medical attention.
Patients taking Wegovy should avoid combining it with:
For patients with type 2 diabetes, using Wegovy alongside insulin or insulin-secreting medications may increase the risk of hypoglycemia (low blood sugar). Healthcare providers may need to adjust insulin dosages to prevent this risk.
Additionally, patients with kidney disease, diabetic retinopathy, or a history of depression should be closely monitored for potential complications.
Wegovy was developed by Novo Nordisk, a pharmaceutical company specializing in diabetes and metabolic disorders. The company previously introduced semaglutide in 2017 under the brand name Ozempic, a lower-dose injection for managing type 2 diabetes. While Ozempic has been widely used off-label for weight loss, Wegovy is the first semaglutide formulation officially approved for chronic weight management at a higher dose.
Wegovy represents a significant advancement in obesity treatment, offering an effective, FDA-approved option for long-term weight loss. Unlike past weight-loss drugs that focused on metabolism or fat absorption, Wegovy targets the neurological regulation of appetite, helping patients control their food intake more effectively.
Clinical trials have demonstrated substantial weight loss, particularly among individuals without diabetes. For those with obesity-related conditions, the drug provides an additional tool to complement diet, exercise, and other medical interventions.
While Wegovy is a promising solution, it is not a standalone cure for obesity. Patients considering the drug should:
The U.S. Food and Drug Administration (FDA) has approved Zepbound (tirzepatide) injection for chronic weight management, marking a significant breakthrough in obesity treatment. The drug is authorized for adults with obesity (BMI ≥ 30 kg/m²) or overweight (BMI ≥ 27 kg/m²) with at least one weight-related condition, such as high blood pressure, type 2 diabetes, or high cholesterol. Zepbound must be used in conjunction with a reduced-calorie diet and increased physical activity to achieve optimal results.
Tirzepatide, the active ingredient in Zepbound, is not new to the medical field. It was previously approved under the brand name Mounjaro for managing blood sugar levels in adults with type 2 diabetes. With its expanded approval for weight management, Zepbound offers a new solution for individuals struggling with obesity and its associated health risks.
Obesity and overweight remain major public health concerns, affecting 70% of U.S. adults. These conditions are closely linked to heart disease, stroke, diabetes, and other life-threatening illnesses.
“Obesity and overweight are serious conditions that can be associated with some of the leading causes of death such as heart disease, stroke, and diabetes,” said John Sharretts, M.D., director of the Division of Diabetes, Lipid Disorders, and Obesity at the FDA. “In light of increasing rates of both obesity and overweight in the United States, today’s approval addresses an unmet medical need.”
Research has shown that losing just 5-10% of body weight through diet and exercise can significantly reduce cardiovascular risks. However, many individuals struggle to achieve and sustain this weight loss, highlighting the need for effective medical interventions.
Zepbound takes a dual-action approach to weight loss by targeting two hormone receptors—GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). These hormones, naturally secreted in the intestine, regulate appetite, calorie intake, and metabolic response. By activating both receptors, Zepbound works to:
The drug is administered as a once-weekly injection, with dosage gradually increasing over 4 to 20 weeks to minimize gastrointestinal side effects. The target maintenance doses include:
The FDA’s approval of Zepbound is based on two major randomized, double-blind, placebo-controlled trials evaluating its impact on weight reduction and maintenance. Together, these studies involved 3,477 participants, including 2,519 patients who received Zepbound and 958 who received placebo injections.
Participants were monitored over 72 weeks, with all Zepbound dosage levels leading to statistically significant weight loss compared to placebo.
These findings underscore Zepbound’s effectiveness in both diabetic and non-diabetic populations, providing a powerful tool for long-term weight management.
Like other medications in its class, Zepbound carries a range of potential side effects, ranging from mild to severe.
Thyroid Cancer Warning:
Other Severe Risks:
Zepbound is not recommended for individuals who:
Healthcare providers should closely monitor patients with kidney disease, diabetic retinopathy, or mental health conditions to ensure safe usage.
The approval of Zepbound marks a significant advancement in the fight against obesity. Unlike older weight-loss medications, it utilizes dual hormone activation to suppress appetite and regulate metabolic function more effectively.
However, Zepbound is not a magic solution. It must be paired with dietary modifications and increased physical activity to deliver sustainable results. Patients should work closely with healthcare providers to monitor progress, manage side effects, and ensure safe long-term use.
Book your weight loss consultation in Fort Lauderdale today and explore the effectiveness of our physician-approved weight loss medication!
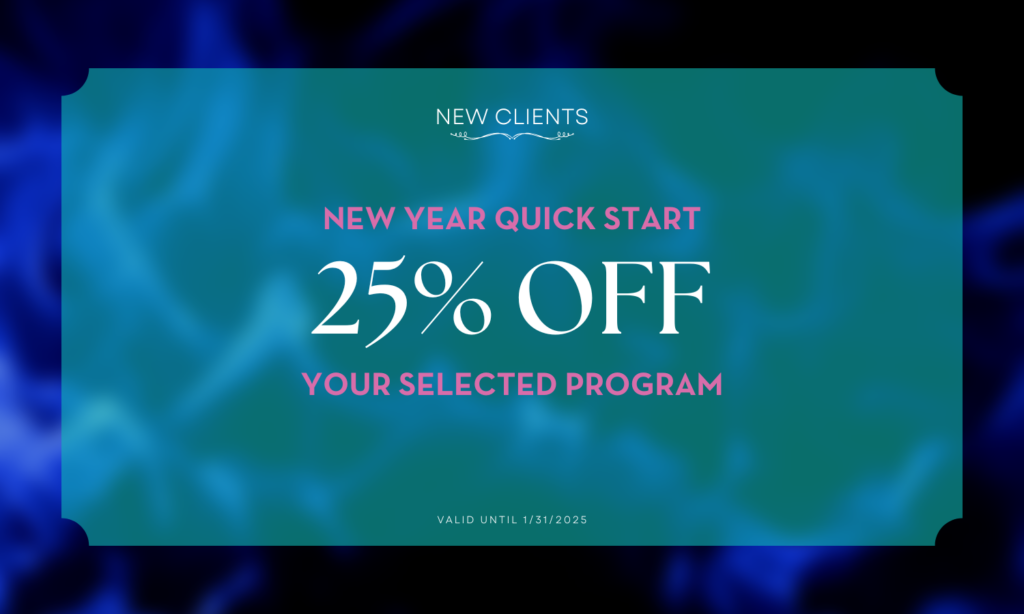
Fill out the form and our team will give you a call!